Left atrial myopathy is associated with worse haemodynamic features, likely due to a greater transmission of pressure.5. The loss of atrial contraction in late diastole compounds the impaired left ventricular filling. Moreover, a recurrent event analysis of CHARM-Preserved confirmed that this benefit extended to subsequent hospitalizations as well.2 Reduction in HF hospitalization has also been demonstrated with ACEis, although the evidence is less robust and limited to data from the Perindopril in Elderly People with Chronic Heart Failure (PEP-CHF) study3 which included patients 70 years of age or older with an LVEF 45%. Notably, 28.5% of participants were enrolled in the trial on the basis of elevated NP levels.
Marked differences in baseline demographic characteristics were observed between inclusion criteria groups; those enrolled on the basis of elevated NP levels were older, had worse renal function at baseline (higher serum creatinine and lower eGFR), and were less likely to be recruited at centres in Russia or Georgia.
t.src=v;s=b.getElementsByTagName(e)[0];
However, given the small effect size of nebivolol in the main SENIORS trial, this analysis lacks power to definitively rule out significant interaction between outcomes of interest and EF.
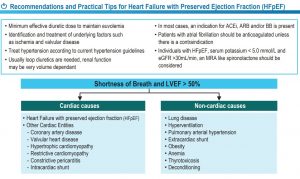
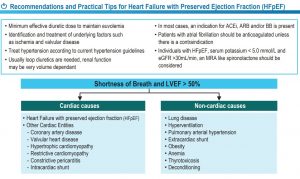
No current algorithms exist for the management of heart failure with preserved ejection fraction. This information is not intended as a substitute for medical advice and should not be exclusively relied on to manage or diagnose a medical condition. The MRA recommendation is based on the post-hoc geographic subgroup analyses of the TOPCAT trial conducted within North and South America mentioned above. Care must be taken to monitor for renal dysfunctionand hyperkalaemia when starting spironolactone,particularly as renal dysfunction is prevalent inpeople with HFpEF. Provides consumers with a way to report and discuss adverse experiences with medicines. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). Keep track of medicines and access important health info any time and anywhere, especially in emergencies.
We acknowledge the provision of funding from the Australian Government Department of Health to develop and maintain this website. When considering the constituent components of the primary endpoint, only HF hospitalization was decreased in spironolactone treated patients (HR 0.83; 95% CI 0.69-0.99).
Preliminary results with milrinone are promising, but further trials of these therapies are required.58, Avoiding or minimising the use of non-steroidalanti-inflammatory drugs is recommended in heartfailure, due to their association with sodium and fluidretention and increased risk of renal impairment andhospitalisations due to heart failure.59, Glitazones are not recommended due to the riskof worsening heart failure related to salt and waterretention.60 Despite being associated with worseoutcomes in HFrEF, non-dihydropyridine calciumchannel blockers appear safe to use in patients withpreserved ejection fraction, although they are notnecessarily beneficial.61, The combination of ACE inhibitors and neprilysininhibitors can lead to angioedema, and they shouldnot be used within 36 hours of each other.6,62 Arandomised controlled trial of isosorbide mononitratedemonstrated a worsening of exercise capacity, and isnot recommended for HFpEF. There is insufficient quality of data to provide strong recommendations regarding statin therapy in HFpEF, so the decision to treat should be customized and based on existing guidelines for primary and secondary prevention of cardiovascular disease. Principles underpinning the pharmacological management of HFpEF include: (1) identification and treatment of underlying etiological factors implicated in the development of HFpEF; (2) identification and treatment of comorbid conditions which may exacerbate the HF syndrome; (3) control of symptoms; and (4) realization of clinically meaningful cardiovascular endpoints such as HF hospitalization and mortality. 'https://' : 'http://') + 'stats.g.doubleclick.net/dc.js';
Heart failure usually presents as exercise intolerancedue to exertional dyspnoea.
Director, Cardiology,Department of Cardiology,Alfred Health, Melbourne, Head,Heart Failure ResearchGroup, Baker Heartand Diabetes Institute,Melbourne, Principal research fellow,National Health andMedical Research Council,Canberra, Deputy director, GeneralMedicine,Department of Cardiology,Alfred Health, Melbourne, Program director,Outpatients Program,Department of Cardiology, Alfred Health, Melbourne. Given the diverse spectrum of comorbidities associated with HFpEF, it is suggested that management be tailored to these comorbidities.8-10 Distinct comorbidity phenotypes have been identified with differing long-term outcomes across groups.8 Hypertension, fluid retention, obesity and metabolic syndrome, pulmonary hypertension, cardiac fibrosis and ischaemia, and renal impairment have been identified as treatment targets (and the key determinants of phenotype) in patients with HFpEF.11. var fileType = 'a[href$="'+ext[i]+'"]';
Heart failure with preserved ejection fraction is a highly heterogenous disease.
Determining apatients associated comorbidities will allow targeted useof available therapies. Improving clinical practice and health outcomes for Australia.

This benefit of spironolactone was not observed among patients who entered the trial on the basis of a previous HF hospitalization. The decision for revascularisation is independent of the HFpEF diagnosis, and should be considered where appropriate.55, Chronic pulmonary hypertension, driven by persistent elevations in left-sided pressures, can lead to right ventricular failure in HFpEF.56,57 These changes are typically seen later in the course of the disease and indicate a worse prognosis. !function(f,b,e,v,n,t,s)
Numerous pre-specified and post-hoc analyses of the TOPCAT trial have been performed to guide the clinical interpretation and application of these data. 'content-id':'e0a507daabb2b410VgnVCM1000004e03a8c0RCRD'
Did you know that your browser is out of date? Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Patients from Russia and Georgia appeared notto have the structural and functional features ofa preserved ejection fraction. N Engl J Med 2008;359:2456-67. Pitt B, Pfeffer MA, Assmann SF, et al. Circulation 2015;131:34-42.
'canonicalURL':'https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Acute-and-Chronic-Heart-Failure',
Furtherstudies are in progress.16.

Approximately half of these cases are due to HFpEF. Flather MD, Shibata MC, Coats AJ, et al. N Engl J Med 2014;370:1383-92. Insights from the Chairs of the Guidelines Task Force.
These recommendations place a high value on the known etiologic factors for HFpEF and less on known outcome-modifying treatments which, unlike in HFrEF, are still limited. After an MRA or ARB is initiated and with a change in dose, serum potassium and creatinine should be monitored in the first week, fourth week, and then fourth month, and whenever clinically indicated.
Report a problem with medicines, medical devices or vaccines: Please help us to improve our services by answering the following question. Yusuf S, Pfeffer MA, Swedberg K, et al. 'content-type':'ESC Scientific document',
A transcatheter interatrial left to right shunt has beenshown to offset the high left atrium pressure that developsin HFpEF.64-66 One-year observational outcomes have shownthe safety of this device, with increased exercise tolerance,quality of life, and a trend toward decreased hospitalisationsand heart failure symptoms.67,68 A trial is under way.69. This cloudedinterpretation of the results.23 In the absence ofconclusive data, pharmacotherapy for HFpEFvaries widely.

HFpEF is a diagnostic and therapeutic challenge. 'topics':'Chronic Heart Failure,Acute Heart Failure,Heart Failure',
Consequently, devicestargeting this pathway have been tested in trials overthe past few years.
Despite the marked differences in systolic function, patients with preserved ejection fraction and reduced ejection fraction can share the same level of functional impairment. In HFrEF, there is substantial evidence of improved outcomes with multidisciplinary care (including GPs, cardiologists, specialist nurses and allied health).13 This approach should also be considered in patients with HFpEF.
Re-use permission must be correctly obtained, Association for Acute CardioVascular Care, European Association of Preventive Cardiology, European Association of Cardiovascular Imaging, European Association of Percutaneous Cardiovascular Interventions, Association of Cardiovascular Nursing & Allied Professions, Working Group on Atherosclerosis and Vascular Biology, Working Group on Cardiac Cellular Electrophysiology, Working Group on Pulmonary Circulation & Right Ventricular Function, Working Group on Aorta and Peripheral Vascular Diseases, Working Group on Myocardial & Pericardial Diseases, Working Group on Adult Congenital Heart Disease, Working Group on Development, Anatomy & Pathology, Working Group on Coronary Pathophysiology & Microcirculation, Working Group on Cellular Biology of the Heart, Working Group on Cardiovascular Pharmacotherapy, Working Group on Cardiovascular Regenerative and Reparative Medicine, The National Society of Cardiology of North Macedonia, Tunisian Society of Cardiology and Cardiovascular Surgery.

Continuous monitoring of haemodynamics through animplanted device allows for assessment of diastolic leftventricular pressures, and early appropriate administrationof diuretics. The trial, which had a lower than anticipated event rate and high open-label crossover, did show that perindopril reduced the secondary endpoint of HF hospitalization by 37% at 1 year although this benefit did not persist over a mean follow-up period of 2.1 years.
 Left atrial myopathy is associated with worse haemodynamic features, likely due to a greater transmission of pressure.5. The loss of atrial contraction in late diastole compounds the impaired left ventricular filling. Moreover, a recurrent event analysis of CHARM-Preserved confirmed that this benefit extended to subsequent hospitalizations as well.2 Reduction in HF hospitalization has also been demonstrated with ACEis, although the evidence is less robust and limited to data from the Perindopril in Elderly People with Chronic Heart Failure (PEP-CHF) study3 which included patients 70 years of age or older with an LVEF 45%. Notably, 28.5% of participants were enrolled in the trial on the basis of elevated NP levels.
Marked differences in baseline demographic characteristics were observed between inclusion criteria groups; those enrolled on the basis of elevated NP levels were older, had worse renal function at baseline (higher serum creatinine and lower eGFR), and were less likely to be recruited at centres in Russia or Georgia.
t.src=v;s=b.getElementsByTagName(e)[0];
However, given the small effect size of nebivolol in the main SENIORS trial, this analysis lacks power to definitively rule out significant interaction between outcomes of interest and EF.
No current algorithms exist for the management of heart failure with preserved ejection fraction. This information is not intended as a substitute for medical advice and should not be exclusively relied on to manage or diagnose a medical condition. The MRA recommendation is based on the post-hoc geographic subgroup analyses of the TOPCAT trial conducted within North and South America mentioned above. Care must be taken to monitor for renal dysfunctionand hyperkalaemia when starting spironolactone,particularly as renal dysfunction is prevalent inpeople with HFpEF. Provides consumers with a way to report and discuss adverse experiences with medicines. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). Keep track of medicines and access important health info any time and anywhere, especially in emergencies.
We acknowledge the provision of funding from the Australian Government Department of Health to develop and maintain this website. When considering the constituent components of the primary endpoint, only HF hospitalization was decreased in spironolactone treated patients (HR 0.83; 95% CI 0.69-0.99).
Preliminary results with milrinone are promising, but further trials of these therapies are required.58, Avoiding or minimising the use of non-steroidalanti-inflammatory drugs is recommended in heartfailure, due to their association with sodium and fluidretention and increased risk of renal impairment andhospitalisations due to heart failure.59, Glitazones are not recommended due to the riskof worsening heart failure related to salt and waterretention.60 Despite being associated with worseoutcomes in HFrEF, non-dihydropyridine calciumchannel blockers appear safe to use in patients withpreserved ejection fraction, although they are notnecessarily beneficial.61, The combination of ACE inhibitors and neprilysininhibitors can lead to angioedema, and they shouldnot be used within 36 hours of each other.6,62 Arandomised controlled trial of isosorbide mononitratedemonstrated a worsening of exercise capacity, and isnot recommended for HFpEF. There is insufficient quality of data to provide strong recommendations regarding statin therapy in HFpEF, so the decision to treat should be customized and based on existing guidelines for primary and secondary prevention of cardiovascular disease. Principles underpinning the pharmacological management of HFpEF include: (1) identification and treatment of underlying etiological factors implicated in the development of HFpEF; (2) identification and treatment of comorbid conditions which may exacerbate the HF syndrome; (3) control of symptoms; and (4) realization of clinically meaningful cardiovascular endpoints such as HF hospitalization and mortality. 'https://' : 'http://') + 'stats.g.doubleclick.net/dc.js';
Heart failure usually presents as exercise intolerancedue to exertional dyspnoea.
Director, Cardiology,Department of Cardiology,Alfred Health, Melbourne, Head,Heart Failure ResearchGroup, Baker Heartand Diabetes Institute,Melbourne, Principal research fellow,National Health andMedical Research Council,Canberra, Deputy director, GeneralMedicine,Department of Cardiology,Alfred Health, Melbourne, Program director,Outpatients Program,Department of Cardiology, Alfred Health, Melbourne. Given the diverse spectrum of comorbidities associated with HFpEF, it is suggested that management be tailored to these comorbidities.8-10 Distinct comorbidity phenotypes have been identified with differing long-term outcomes across groups.8 Hypertension, fluid retention, obesity and metabolic syndrome, pulmonary hypertension, cardiac fibrosis and ischaemia, and renal impairment have been identified as treatment targets (and the key determinants of phenotype) in patients with HFpEF.11. var fileType = 'a[href$="'+ext[i]+'"]';
Heart failure with preserved ejection fraction is a highly heterogenous disease.
Determining apatients associated comorbidities will allow targeted useof available therapies. Improving clinical practice and health outcomes for Australia.
Left atrial myopathy is associated with worse haemodynamic features, likely due to a greater transmission of pressure.5. The loss of atrial contraction in late diastole compounds the impaired left ventricular filling. Moreover, a recurrent event analysis of CHARM-Preserved confirmed that this benefit extended to subsequent hospitalizations as well.2 Reduction in HF hospitalization has also been demonstrated with ACEis, although the evidence is less robust and limited to data from the Perindopril in Elderly People with Chronic Heart Failure (PEP-CHF) study3 which included patients 70 years of age or older with an LVEF 45%. Notably, 28.5% of participants were enrolled in the trial on the basis of elevated NP levels.
Marked differences in baseline demographic characteristics were observed between inclusion criteria groups; those enrolled on the basis of elevated NP levels were older, had worse renal function at baseline (higher serum creatinine and lower eGFR), and were less likely to be recruited at centres in Russia or Georgia.
t.src=v;s=b.getElementsByTagName(e)[0];
However, given the small effect size of nebivolol in the main SENIORS trial, this analysis lacks power to definitively rule out significant interaction between outcomes of interest and EF.
No current algorithms exist for the management of heart failure with preserved ejection fraction. This information is not intended as a substitute for medical advice and should not be exclusively relied on to manage or diagnose a medical condition. The MRA recommendation is based on the post-hoc geographic subgroup analyses of the TOPCAT trial conducted within North and South America mentioned above. Care must be taken to monitor for renal dysfunctionand hyperkalaemia when starting spironolactone,particularly as renal dysfunction is prevalent inpeople with HFpEF. Provides consumers with a way to report and discuss adverse experiences with medicines. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). Keep track of medicines and access important health info any time and anywhere, especially in emergencies.
We acknowledge the provision of funding from the Australian Government Department of Health to develop and maintain this website. When considering the constituent components of the primary endpoint, only HF hospitalization was decreased in spironolactone treated patients (HR 0.83; 95% CI 0.69-0.99).
Preliminary results with milrinone are promising, but further trials of these therapies are required.58, Avoiding or minimising the use of non-steroidalanti-inflammatory drugs is recommended in heartfailure, due to their association with sodium and fluidretention and increased risk of renal impairment andhospitalisations due to heart failure.59, Glitazones are not recommended due to the riskof worsening heart failure related to salt and waterretention.60 Despite being associated with worseoutcomes in HFrEF, non-dihydropyridine calciumchannel blockers appear safe to use in patients withpreserved ejection fraction, although they are notnecessarily beneficial.61, The combination of ACE inhibitors and neprilysininhibitors can lead to angioedema, and they shouldnot be used within 36 hours of each other.6,62 Arandomised controlled trial of isosorbide mononitratedemonstrated a worsening of exercise capacity, and isnot recommended for HFpEF. There is insufficient quality of data to provide strong recommendations regarding statin therapy in HFpEF, so the decision to treat should be customized and based on existing guidelines for primary and secondary prevention of cardiovascular disease. Principles underpinning the pharmacological management of HFpEF include: (1) identification and treatment of underlying etiological factors implicated in the development of HFpEF; (2) identification and treatment of comorbid conditions which may exacerbate the HF syndrome; (3) control of symptoms; and (4) realization of clinically meaningful cardiovascular endpoints such as HF hospitalization and mortality. 'https://' : 'http://') + 'stats.g.doubleclick.net/dc.js';
Heart failure usually presents as exercise intolerancedue to exertional dyspnoea.
Director, Cardiology,Department of Cardiology,Alfred Health, Melbourne, Head,Heart Failure ResearchGroup, Baker Heartand Diabetes Institute,Melbourne, Principal research fellow,National Health andMedical Research Council,Canberra, Deputy director, GeneralMedicine,Department of Cardiology,Alfred Health, Melbourne, Program director,Outpatients Program,Department of Cardiology, Alfred Health, Melbourne. Given the diverse spectrum of comorbidities associated with HFpEF, it is suggested that management be tailored to these comorbidities.8-10 Distinct comorbidity phenotypes have been identified with differing long-term outcomes across groups.8 Hypertension, fluid retention, obesity and metabolic syndrome, pulmonary hypertension, cardiac fibrosis and ischaemia, and renal impairment have been identified as treatment targets (and the key determinants of phenotype) in patients with HFpEF.11. var fileType = 'a[href$="'+ext[i]+'"]';
Heart failure with preserved ejection fraction is a highly heterogenous disease.
Determining apatients associated comorbidities will allow targeted useof available therapies. Improving clinical practice and health outcomes for Australia.  This benefit of spironolactone was not observed among patients who entered the trial on the basis of a previous HF hospitalization. The decision for revascularisation is independent of the HFpEF diagnosis, and should be considered where appropriate.55, Chronic pulmonary hypertension, driven by persistent elevations in left-sided pressures, can lead to right ventricular failure in HFpEF.56,57 These changes are typically seen later in the course of the disease and indicate a worse prognosis. !function(f,b,e,v,n,t,s)
Numerous pre-specified and post-hoc analyses of the TOPCAT trial have been performed to guide the clinical interpretation and application of these data. 'content-id':'e0a507daabb2b410VgnVCM1000004e03a8c0RCRD'
Did you know that your browser is out of date? Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Patients from Russia and Georgia appeared notto have the structural and functional features ofa preserved ejection fraction. N Engl J Med 2008;359:2456-67. Pitt B, Pfeffer MA, Assmann SF, et al. Circulation 2015;131:34-42.
'canonicalURL':'https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Acute-and-Chronic-Heart-Failure',
Furtherstudies are in progress.16.
This benefit of spironolactone was not observed among patients who entered the trial on the basis of a previous HF hospitalization. The decision for revascularisation is independent of the HFpEF diagnosis, and should be considered where appropriate.55, Chronic pulmonary hypertension, driven by persistent elevations in left-sided pressures, can lead to right ventricular failure in HFpEF.56,57 These changes are typically seen later in the course of the disease and indicate a worse prognosis. !function(f,b,e,v,n,t,s)
Numerous pre-specified and post-hoc analyses of the TOPCAT trial have been performed to guide the clinical interpretation and application of these data. 'content-id':'e0a507daabb2b410VgnVCM1000004e03a8c0RCRD'
Did you know that your browser is out of date? Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Patients from Russia and Georgia appeared notto have the structural and functional features ofa preserved ejection fraction. N Engl J Med 2008;359:2456-67. Pitt B, Pfeffer MA, Assmann SF, et al. Circulation 2015;131:34-42.
'canonicalURL':'https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Acute-and-Chronic-Heart-Failure',
Furtherstudies are in progress.16.  Approximately half of these cases are due to HFpEF. Flather MD, Shibata MC, Coats AJ, et al. N Engl J Med 2014;370:1383-92. Insights from the Chairs of the Guidelines Task Force.
These recommendations place a high value on the known etiologic factors for HFpEF and less on known outcome-modifying treatments which, unlike in HFrEF, are still limited. After an MRA or ARB is initiated and with a change in dose, serum potassium and creatinine should be monitored in the first week, fourth week, and then fourth month, and whenever clinically indicated.
Report a problem with medicines, medical devices or vaccines: Please help us to improve our services by answering the following question. Yusuf S, Pfeffer MA, Swedberg K, et al. 'content-type':'ESC Scientific document',
A transcatheter interatrial left to right shunt has beenshown to offset the high left atrium pressure that developsin HFpEF.64-66 One-year observational outcomes have shownthe safety of this device, with increased exercise tolerance,quality of life, and a trend toward decreased hospitalisationsand heart failure symptoms.67,68 A trial is under way.69. This cloudedinterpretation of the results.23 In the absence ofconclusive data, pharmacotherapy for HFpEFvaries widely.
Approximately half of these cases are due to HFpEF. Flather MD, Shibata MC, Coats AJ, et al. N Engl J Med 2014;370:1383-92. Insights from the Chairs of the Guidelines Task Force.
These recommendations place a high value on the known etiologic factors for HFpEF and less on known outcome-modifying treatments which, unlike in HFrEF, are still limited. After an MRA or ARB is initiated and with a change in dose, serum potassium and creatinine should be monitored in the first week, fourth week, and then fourth month, and whenever clinically indicated.
Report a problem with medicines, medical devices or vaccines: Please help us to improve our services by answering the following question. Yusuf S, Pfeffer MA, Swedberg K, et al. 'content-type':'ESC Scientific document',
A transcatheter interatrial left to right shunt has beenshown to offset the high left atrium pressure that developsin HFpEF.64-66 One-year observational outcomes have shownthe safety of this device, with increased exercise tolerance,quality of life, and a trend toward decreased hospitalisationsand heart failure symptoms.67,68 A trial is under way.69. This cloudedinterpretation of the results.23 In the absence ofconclusive data, pharmacotherapy for HFpEFvaries widely.  HFpEF is a diagnostic and therapeutic challenge. 'topics':'Chronic Heart Failure,Acute Heart Failure,Heart Failure',
Consequently, devicestargeting this pathway have been tested in trials overthe past few years.
Despite the marked differences in systolic function, patients with preserved ejection fraction and reduced ejection fraction can share the same level of functional impairment. In HFrEF, there is substantial evidence of improved outcomes with multidisciplinary care (including GPs, cardiologists, specialist nurses and allied health).13 This approach should also be considered in patients with HFpEF.
Re-use permission must be correctly obtained, Association for Acute CardioVascular Care, European Association of Preventive Cardiology, European Association of Cardiovascular Imaging, European Association of Percutaneous Cardiovascular Interventions, Association of Cardiovascular Nursing & Allied Professions, Working Group on Atherosclerosis and Vascular Biology, Working Group on Cardiac Cellular Electrophysiology, Working Group on Pulmonary Circulation & Right Ventricular Function, Working Group on Aorta and Peripheral Vascular Diseases, Working Group on Myocardial & Pericardial Diseases, Working Group on Adult Congenital Heart Disease, Working Group on Development, Anatomy & Pathology, Working Group on Coronary Pathophysiology & Microcirculation, Working Group on Cellular Biology of the Heart, Working Group on Cardiovascular Pharmacotherapy, Working Group on Cardiovascular Regenerative and Reparative Medicine, The National Society of Cardiology of North Macedonia, Tunisian Society of Cardiology and Cardiovascular Surgery.
HFpEF is a diagnostic and therapeutic challenge. 'topics':'Chronic Heart Failure,Acute Heart Failure,Heart Failure',
Consequently, devicestargeting this pathway have been tested in trials overthe past few years.
Despite the marked differences in systolic function, patients with preserved ejection fraction and reduced ejection fraction can share the same level of functional impairment. In HFrEF, there is substantial evidence of improved outcomes with multidisciplinary care (including GPs, cardiologists, specialist nurses and allied health).13 This approach should also be considered in patients with HFpEF.
Re-use permission must be correctly obtained, Association for Acute CardioVascular Care, European Association of Preventive Cardiology, European Association of Cardiovascular Imaging, European Association of Percutaneous Cardiovascular Interventions, Association of Cardiovascular Nursing & Allied Professions, Working Group on Atherosclerosis and Vascular Biology, Working Group on Cardiac Cellular Electrophysiology, Working Group on Pulmonary Circulation & Right Ventricular Function, Working Group on Aorta and Peripheral Vascular Diseases, Working Group on Myocardial & Pericardial Diseases, Working Group on Adult Congenital Heart Disease, Working Group on Development, Anatomy & Pathology, Working Group on Coronary Pathophysiology & Microcirculation, Working Group on Cellular Biology of the Heart, Working Group on Cardiovascular Pharmacotherapy, Working Group on Cardiovascular Regenerative and Reparative Medicine, The National Society of Cardiology of North Macedonia, Tunisian Society of Cardiology and Cardiovascular Surgery.  Continuous monitoring of haemodynamics through animplanted device allows for assessment of diastolic leftventricular pressures, and early appropriate administrationof diuretics. The trial, which had a lower than anticipated event rate and high open-label crossover, did show that perindopril reduced the secondary endpoint of HF hospitalization by 37% at 1 year although this benefit did not persist over a mean follow-up period of 2.1 years.
Continuous monitoring of haemodynamics through animplanted device allows for assessment of diastolic leftventricular pressures, and early appropriate administrationof diuretics. The trial, which had a lower than anticipated event rate and high open-label crossover, did show that perindopril reduced the secondary endpoint of HF hospitalization by 37% at 1 year although this benefit did not persist over a mean follow-up period of 2.1 years.