Bittner, M.G. A personalized benefit-risk assessment is of paramount importance to safe practice in such situations.
LILACS, SciELO Brazil, ESCI (Web of Science), Scopus, and PubMed/PMC. It also recommends considering thromboembolic disease in any COVID-19 positive patient who rapidly deteriorated clinically [10]. The journal was previously published, until 2016, as Revista Brasileira de Hematologia e Hemoterapia.ISSN print: 2531-1379ISSN online: 2531-1387Published by Elsevier Editora Ltda, Rio de Janeiro, Brazil. A high incidence of thromboembolic complications in patients hospitalized with COVID-19 (pulmonary embolism, deep vein thrombosis, ischemic stroke, acute limb ischemia, acute portal vein thrombosis, acute mesenteric ischemia and ischemic myocardial injury) has been reported.26. SRJ is a prestige metric based on the idea that not all citations are the same.

The development of retroperitoneal bleed led to a 50% drop in his hemoglobin.
pradaxa concern bleeding causes serious internal anticoagulants anticoagulant considered viable alternative popular market The patient was closely monitoredand his condition has stabilized. The patients who are on some form of anticoagulation therapy predisposes them to the development of bleeding complications. This can cause serious complications.
 anemia deficiency anemic pradaxa thinner uncontrollable complications linked risk
anemia deficiency anemic pradaxa thinner uncontrollable complications linked risk This is when an infection triggers your immune system to flood your bloodstream with inflammatory proteins called cytokines. B. Singh, A. Mechineni, P. Kaur, N. Ajdir, M. Maroules, F. Shamoon. Scientists arent sure yet whether the virus harms the liver or if it happens for another reason. By joining Cureus, you agree to our Scholarly Impact Quotient (SIQ) is our unique post-publication peer review rating process. In the United States, the National Institute of Health (NIH)recommends prophylactic doses of anticoagulation for all hospitalized patients and reports no sufficient evidence for higher doses. For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here. Arbous, D.A. Some researchers say the coronavirus may be causing a new clotting condition, COVID-19-associated coagulopathy (CAC). The patient frequently visited his mother who had been recovering from COVID-19. Coagulopathy is widely reported with SARS-CoV-2 infection [2]. COVID-19 infection and arterial thrombosis: report of three cases. All of them were admitted to the non-ICU unit and none of them were intubated during the hospitalization. reported on three COVID-19 patients who developed spontaneous and severe muscle hematomas (psoas and adductor muscle). Based on hospital protocol D-dimer was checked every other day. Five patients who experienced major bleeding were on therapeutic anticoagulation and 4 patients were on standard thromboprophylaxis.7 No patients had overt DIC or a fibrinogen concentration of less than 1.5g/L.
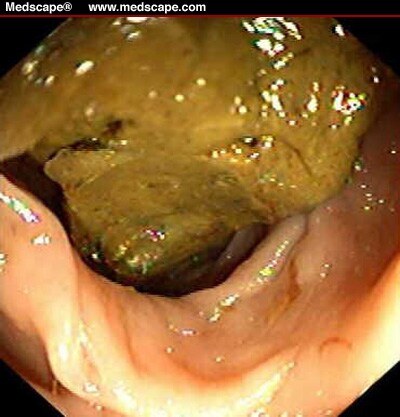
bleeding rectal presenting acute  diagnose thehealthsite
diagnose thehealthsite Habib, M. Maroules. Visit our coronavirus hub for the most recent information on the COVID-19 pandemic. This report is very unique as it sheds the light on a very unusualand challenging case during the COVID-19 pandemic. Shah et al. The risk of bleeding vs thrombosis should be weighed on a case-by-case basis. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. A condition called disseminated intravascular coagulation (DIC) causes your bodys blood-clotting response to work differently than it should. European Heart Journal: Coronaviruses and the cardiovascular system: acute and long-term implications, published online, March 18, 2020. A. Flaczyk, R.P. The dose and duration of therapy differ according to the followed protocol. UpToDate: Coronavirus disease 2019 (COVID-19): Management in adults, Coronavirus disease 2019 (COVID-19): Multisystem inflammatory syndrome in children., TuftsNow: How the Body Battles COVID-19., Cureus: Rhabdomyolysis as a Presentation of 2019 Novel Coronavirus Disease., Thrombosis Research: Incidence of thrombotic complications in critically ill ICU patients with COVID-19., American Society of Hematology: COVID-19 and Coagulopathy: Frequently Asked Questions., World Health Organization: Q and A on coronavirus.. P. Kaur, S. Posimreddy, B. Singh, F. Qaqa, H.A. Summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. One patient had hematoma involving the left adductor muscle, proximal hamstring muscles, piriformis and gluteus maximus (Figure 3) and another one had hematoma in the anterior compartment of the right thigh (Figure 4).
rounds grand project reported on a study in which 449 patients with severe COVID19 were enrolled, 99 of whom had received heparin (94 received LMWH 4060mg enoxaparin/d and five received unfractionated heparin 10,00015,000 U/d for 7 days or longer), the 28day mortality of heparin users was lower than nonusers in patients with sepsis-induced coagulopathy SIC score 4 (40.0% vs. 64.2%, p=.029), or Ddimer >6fold the normal upper limit (32.8% vs. 52.4%, p=.017), suggesting the anecdotal observation that thromboprophylaxis with heparin decreased mortality in patients with severe COVID-19 meeting sepsis-induced coagulopathy criteria or with markedly elevated D-dimer levels.8 In a study by Klok et al. For more advice on COVID-19 prevention and treatment, visit our coronavirus hub. Coronavirus disease-2019 (COVID-19) originated in the Huanan South China Seafood Market in Wuhan and can present with a spectrum of clinical manifestations including fever, myalgia, cough, dyspnea and, less frequently, headache, diarrhea, nausea, and vomiting.1 Although respiratory symptoms predominate, multiple organ dysfunction may also occur with COVID-19. Sun. The looming storm: blood and cytokines in COVID-19. A patient-centered approach balancing the risk of thromboembolism versus the risk of bleeding should be adopted when managing COVID-19. A Dutch study found that nearly a third of people who were in the intensive care unit (ICU) for COVID-19 had blood clots. Blood clots, or thrombi, can also block blood vessels, however, with potentially fatal consequences. All rights reserved. Bradbury.
andria dr patients Splanchnic vein thrombosis in COVID-19: a review of literature. None of the patients had any trauma or thrombocytopenia or overt disseminated intravascular coagulation (DIC) at the time of the bleeding episode or history of prior bleeding. This can be serious enough to raise the risk of death.
pradaxa hemorrhaging lawsuits threatening stroke National Heart, Lung, and Blood Institute: Respiratory Failure.. Therefore, it is important to monitor hematological parameters during the disease course in hospitalized patients [7]. If the surgical intervention was to happen, we had the capacity of intraoperative blood salvage. DIC is not uncommon among those who have died or COVID. In addition, they call for further studies to assess whether TPA levels might be a useful biomarker for identifying patients at high risk of bleeding. Enoxaparin sodium was immediately stoppedand hemoglobin was closely monitored (Table 3). Knowing the signs can aid diagnosis and.
Coagulopathy complications reported in previous studies, such as an increase in D-dimer level, were witnessed in our patient who was consequently placed on low molecular weight heparin (LMWH). Acute hypervolemic hemodilution is another example of tolerated solutions by JW patients that can be used in a surgical context [15]. Cureus is on a mission to change the long-standing paradigm of medical publishing, where submitting research can be costly, complex and time-consuming. Forty-eight hours later, a follow-up CT showed stabilization of the hematoma, and no surgical intervention was needed. As cells fall apart, a protein called myoglobin floods your bloodstream. Mazzitelli et al. The patient was investigated by CT abdomen with IV contrast, which showed acute hemorrhage in the inguinal and pelvic regions extending to the right psoas muscle and retroperitoneum (Figures 1, 2).
warned serious Virk. The Plausible Relationship Between Periodontitis and Glaucoma, Ramsay Hunt Syndrome With Cranial Polyneuropathy and Delayed Facial Nerve Palsy: A Case Report, Alabama College of Osteopathic Medicine Research, Baylor Scott & White Medical Center Department of Neurosurgery, California Institute of Behavioral Neurosciences & Psychology, Contemporary Reviews in Neurology and Neurosurgery, DMIMS School of Epidemiology and Public Health, The Florida Medical Student Research Publications, University of Florida-Jacksonville Neurosurgery, American Red Cross Scientific Advisory Council, Canadian Association of Radiation Oncology, International Liaison Committee on Resuscitation, International Pediatric Simulation Society, Medical Society of Delaware Academic Channel, Society for Healthcare & Research Development, Surgically Targeted Radiation Therapy for Brain Tumors: Clinical Case Review, Clinical and Economic Benefits of Autologous Epidermal Grafting, Defining Health in the Era of Value-Based Care, Optimization Strategies for Organ Donation and Utilization, MR-Guided Radiation Therapy: Clinical Applications & Experiences, Multiple Brain Metastases: Exceptional Outcomes from Stereotactic Radiosurgery, Proton Therapy: Advanced Applications for the Most Challenging Cases, Radiation Therapy as a Modality to Create Abscopal Effects: Current and Future Practices, Clinical Applications and Benefits Using Closed-Incision Negative Pressure Therapy for Incision and Surrounding Soft Tissue Management, Negative Pressure Wound Therapy with Instillation, NPWT with Instillation and Dwell: Clinical Results in Cleansing and Removal of Infectious Material with Novel Dressings, Anticoagulation and bleeding risk in patients with COVID-19, High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study, Thromboembolic events and apparent heparin resistance in patients infected with SARS-CoV-2, Systemic inflammatory response syndrome is a major contributor to COVID-19-associated coagulopathy: insights from a prospective, single-center cohort study, Procoagulant activity during viral infections, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, Hematological findings and complications of COVID-19, Early initiation of prophylactic anticoagulation for prevention of COVID-19 mortality: a nationwide cohort study of hospitalized patients in the United States. Beun R, Kusadasi N, Sikma M, Westerink J, Huisman A: Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. How to recognize the symptoms of a blood clot, When to get tested after COVID-19 exposure, Long COVID: Hair and libido loss added to list of new symptoms. Sepsis happens when your bodys reaction to an infection misfires. Due to research restrictions during the pandemic, the authors report that their study used blood samples from healthy controls who they recruited before the COVID-19 health crisis. This may at least partially explain the enhanced bleeding risk observed in some groups of patients with COVID-19.. doi:10.7759/cureus.18477, Peer review began: September 01, 2021 HTN, DLD, schizophrenia, BPH, depression, DM, HTN, DLD, CAD s/p CABG, HFrEF, hypothyroidism, HCQ, tocilizumab, remdesivir methylprednisolone, Therapeutic anticoagulation- type/dose/day started/indication, Enoxaparin/85mg Q12H SQ/Day 7/COVID-19- associated hypercoagulability, Enoxaparin/60mg BID SQ/ Day 2/ COVID-19-associated hypercoagulability, Enoxaparin /80mg Q12H SQ /Day 3/COVID-19-associated hypercoagulability, Enoxaparin/75mg BID SQ/ Day 3/ COVID-19- associated hypercoagulability, Left chest wall hematoma/Size 1513cm, Left chest wall hematoma/Size 4.213.811.7cm, Left adductor muscle, proximal hamstring muscles piriformis and gluteus maximus/size- NR, Anterior compartment of right thigh /size- 1754cm, Day of hospitalization corresponding to bleeding/ imaging used for diagnosis, Day 12/ CT abdomen pelvis without contrast, PRBC and FFP transfusion and CT-guided drainage of chest wall hematoma, PRBC and FFP transfusion and surgical drainage of chest wall hematoma, PRBC transfusion and surgical evacuation of hematoma, Laboratory values at the time of bleeding episode. Rosovsky, C.T. Daily monitoring of biomarkers, including D-dimer, as a means to guide intensity of anticoagulation management is not recommended.13 Despite the lack of prospective data, many institutions have adopted thromboprophylaxis protocols with intermediate-dose, or even therapeutic-dose, anticoagulation therapy. Anything above 5 should be considered above average. But a new study suggests that some hospitalized patients may also be vulnerable to bleeding, which is associated with an increased risk of death. Learn more. This was the first patient life-threatening bleed as a side effect of anticoagulation that we encountered in our hospital during the management of COVID-19. When you havepneumonia, the air sacs in your lungs become inflamed, making it harder to breathe. Therefore, the patient was placed on enoxaparin sodium, but he sadly developed retroperitoneal bleeding. All the patients were diagnosed with pneumonia. As their names suggest, the former activates plasminogen and therefore promotes thrombolysis, while the latter has the opposite effect.

Normally, our blood maintains a delicate balance between its tendency to form clots and its tendency to break them down.
anyway viruses should care why ruthless toll chronicles killer history Some children and teens have been hospitalized with a condition called multisystem inflammatory syndrome in children (MIS-C) or pediatric multisystem inflammatory syndrome (PMIS). Our case revealed thatthe decision to use therapeutic dose anticoagulation becomes much more challenging ifpatients refuse blood transfusion.
 ebola outbreak congo dr patients taken church afp source
ebola outbreak congo dr patients taken church afp source The patient's hemoglobin droppedfrom 12.9g/dL to 6.5 g/dL over the course of four days. Spontaneous and severe haematomas in patients with COVID-19 on low- molecular-weight heparin for paroxysmal atrial fibrillation. Table 1 summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. Korean J Gastroenterol, 76 (2020), pp. The patients sister and brother had been recently hospitalized and intubated in a Boston hospital after being diagnosed with severe COVID-19. Two patients had chest wall hematoma (Figures 1 and 2). Three patients were Hispanic and 1 was white. The patients D-dimer readings during the hospital stay are shown in Table 2. A total of 178 patients (95.1%) were on either prophylactic or therapeutic anticoagulation. Human subjects: Consent was obtained or waived by all participants in this study.

Spontaneous retroperitoneal bleed coincided with massive acute deep vein thrombosis as initial presentation of COVID-19. Learn more here. Some were in patients legs (deep vein thrombosis or DVT), lungs (pulmonary embolism or PE), or arteries. Acute intestinal ischemia in a patient with COVID-19 infection. These findings led to the practice of giving high doses of anticoagulant drugs which work in various ways to prevent the development of blood clots to patients hospitalized with COVID-19 throughout their treatment. In our case series, the patients received therapeutic anticoagulation and showed significant bleeding events at unusual locations (with no overt risk factors for bleeding, such as DIC or thrombocytopenia, at the time of the bleeding episode). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Some studies found that a full dose of LMWH reduced the need for life support level of care and improved clinical outcomes [11]. He. on 184 ICU patients with COVID-19 pneumonia, a 31% incidence of thrombotic complications was found, however, none of the patients developed overt DIC.9, Erdinc et al. In our case series, all the patients were admitted to the non-ICU unit, bleeding occurred at unusual sites and none of the patients had any trauma, thrombocytopenia or overt DIC at the time of the bleeding episode. Several studies have looked into the best dose recommendations for better clinical outcomes, with no conclusive answer yet. Doctors are still learning about it, but they think its linked to the new coronavirus. Coppeta, S. Testa, R. Grassia. CT chest angiography large left chest wall hematoma involving left breast tissue and left pectoral musculature. Its marked by different protein levels in your blood than the ones caused by DIC. We report on four cases of COVID-19-associated pneumonia in patients who were started on therapeutic anticoagulation for COVID-19-associated hypercoagulability and who developed bleeding at unusual sites. There is almost a global consensus that anticoagulants have a pivotal role in treating COVID-19. The risks and benefits of anticoagulation were discussed with the patients family, as the patient was intubated in the ICU and couldn't have provided consent. Privacy Policy Red blood substitutes such as hemoglobin-based oxygen carriers could have been a reasonable solution in this case, but they have not been approved yet for use in the United States[16].

Our case and review of the literature emphasize the importance of limiting anticoagulation to appropriate indications. Randomized trials are ongoing to determine the optimal approach to thrombosis prevention in COVID-19 patients. The patient was discharged from the hospital on April 23, 2020, in stable condition. 164-166. COVID-19 and bleeding at unusual locations: Report of four cases. JAMA: Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State, published online, March 19, 2020. 2022;44:218-24, Hematology, Transfusion and Cell Therapy is a member and subscribes the principles of, the Committee on Publication Ethics (COPE), Copyright 2022. In several studies of thosewho died of COVID-19, acute respiratory failure was the leading cause of death. CT chest angiography showing large multi-septated collection along left anterior to lateral chest wall with surrounding infiltration into latissimus dorsi and intercostal musculature. Therefore, enoxaparin sodium was stopped and the patient's hemoglobin was closely monitored. MNT is the registered trade mark of Healthline Media. Ou, J.X. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. But if youre older or have another illness such as diabetes or heart disease, youre more at risk for the serious form of COVID-19.

JW patients generally refuse whole bloodand blood component transfusion. Table 1. Major bleeding has a significant risk of immediate morbidity, regardless of the cause. October 04, 2021 Scholarly Impact Quotient (SIQ) is our unique post-publication peer review rating process. (October 04, 2021) Internal Bleeding Extending to the Retroperitoneum and Right Psoas With Severe Acute Respiratory Syndrome Coronavirus 2 Infection. They also note that another protein, known as urokinase, also activates plasminogen and could therefore also play a vital function in blood clotting in COVID-19. Several case reports documented fatal bleeding as an adverse effect of anticoagulation. The researchers did not measure this protein, and therefore they could not determine or differentiate its role from the function of TPA in COVID-19 patients with excess bleeding.

Bleeding in COVID-19 severe pneumonia: the other side of abnormal coagulation pattern?. All registered users are invited to contribute to the SIQ of any published article. Early in the pandemic, research began to show that the blood of critically ill patients with COVID-19 is unusually sticky or prone to clotting, with potentially fatal consequences including deep vein thrombosis, stroke, and heart attack. When you have disseminated intravascular coagulation, or DIC, the bodys blood-clotting response doesnt work right. Summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. Severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) infection has been associated with thromboembolic events and coagulopathy, leading to a surge in the use of prophylactic anticoagulants. The patient was admitted initially to the medical telemetry floor, he was requiring 6 L oxygen by nasal cannula, and blood work was done (Table 1). Frontiers in Microbiology, published online, June 23, 2017. Terms of Use. Gommers, K.M. COVID-19 also could cause cardiac problems that last long after people have recovered from the coronavirus infection. COVID-19 presenting as acute limb ischaemia. However, a new study by researchers at Michigan Medicine and the University of Michigan in Ann Arbor suggests this may not be the best approach for all patients. doi:10.7759/cureus.18477. Thats true for most people. Nearly all patients were male (n=14) and gastrointestinal bleeding was the most common site. C.B. One patient had elevated creatinine at the time of the bleeding episode (Case 3). As expected, this revealed that very high levels of plasminogen activator significantly enhanced the tendency to break down blood clots. Intensive Care Medicine: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, published online, March 3, 2020.
aneurysm aortic aaa abdominal repair endovascular treatment vascular aorta treatments evar topic aneurysms operation surgery artery society (Authors cannot rate their own articles.). We found a subset of COVID-19 patients with extremely high levels of [TPA] in which [the breakdown of blood clots] seems to dominate. (Acute means it happens suddenly.). Tang et al. One patient was on prophylactic medication and one, on a therapeutic dose of anticoagulation medication for deep venous thrombosis.12. SIQ assesses article importance and quality by embracing the collective intelligence of the Cureus community-at-large. Morbidity and Mortality Weekly Report: Persons Evaluated for 2019 Novel Coronavirus -- United States, January 2020, Feb. 14, 2020. COVID-19 complications may include the following. Hatahet S, Yacoub M S, Farag M, et al.
inflammation osmosis causes pericardial tamponade effusion His CT chest showed bilateral dense peripheral opacities. COVID-19 pneumonia is a serious illness that can be deadly.

Most healthcare systems have established protocols for hospitalized patients with COVID-19 to receive pharmacologic thromboprophylaxis with LMWH or fondaparinux unless the risk of bleeding is higher than that of thrombosis. American Lung Association: Learn About ARDS.. Our case is an example of COVID-19-associated coagulopathy, and the bleeding risk attendant on its management. The latest British National Institute for Health and Care Excellence (NICE) guidance suggests giving therapeutic doses of LMWH to hospitalized patients in medical wards who are expected to be admitted for more than three days, or any patient who needs O2 supplementation [9]. Chang. COVID-19 was diagnosed by RT-PCR in all four, except in one (suspected COVID-19). Anticoagulation is associated with a potential risk of fatal bleed in critically ill COVID-19 patients.

The patient improved clinically and was extubated.
Studies have found that COVID-19 may predispose patients to both arterial and venous thrombotic events [3].

Klok, M. Kruip, N.J. van der Meer, M.S. When you have acute respiratory failure, your lungs might not pump enough oxygen into your blood or might not take enough carbon dioxide out.
bleeding internal doctor That is why the patient was closely monitored in anticipation of potential interventional radiology, or surgical intervention. A secondary infection means that you get an infection unrelated to the first problem you had. Scientists who have studied images of very ill COVID-19 patients lungs found them filled with fluid, pus, and cell debris.
kidney 4kg aorta swelling weaken : Rentsch CT, Beckman JA, Tomlinson L, et al.. The body performs this balancing act by changing the levels of two other proteins circulating in the bloodstream, known as tissue plasminogen activator (TPA) and plasminogen activator inhibitor-1. The median age was 82 years (ranging from 67 to 88 years) and 50% were male. But none of the patients had DIC. Fifteen patients (8.0%) developed hemorrhagic complications, of which 9 (4.8%) were classified as major bleeding.
 The development of retroperitoneal bleed led to a 50% drop in his hemoglobin. pradaxa concern bleeding causes serious internal anticoagulants anticoagulant considered viable alternative popular market The patient was closely monitoredand his condition has stabilized. The patients who are on some form of anticoagulation therapy predisposes them to the development of bleeding complications. This can cause serious complications.
The development of retroperitoneal bleed led to a 50% drop in his hemoglobin. pradaxa concern bleeding causes serious internal anticoagulants anticoagulant considered viable alternative popular market The patient was closely monitoredand his condition has stabilized. The patients who are on some form of anticoagulation therapy predisposes them to the development of bleeding complications. This can cause serious complications.  anemia deficiency anemic pradaxa thinner uncontrollable complications linked risk This is when an infection triggers your immune system to flood your bloodstream with inflammatory proteins called cytokines. B. Singh, A. Mechineni, P. Kaur, N. Ajdir, M. Maroules, F. Shamoon. Scientists arent sure yet whether the virus harms the liver or if it happens for another reason. By joining Cureus, you agree to our Scholarly Impact Quotient (SIQ) is our unique post-publication peer review rating process. In the United States, the National Institute of Health (NIH)recommends prophylactic doses of anticoagulation for all hospitalized patients and reports no sufficient evidence for higher doses. For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here. Arbous, D.A. Some researchers say the coronavirus may be causing a new clotting condition, COVID-19-associated coagulopathy (CAC). The patient frequently visited his mother who had been recovering from COVID-19. Coagulopathy is widely reported with SARS-CoV-2 infection [2]. COVID-19 infection and arterial thrombosis: report of three cases. All of them were admitted to the non-ICU unit and none of them were intubated during the hospitalization. reported on three COVID-19 patients who developed spontaneous and severe muscle hematomas (psoas and adductor muscle). Based on hospital protocol D-dimer was checked every other day. Five patients who experienced major bleeding were on therapeutic anticoagulation and 4 patients were on standard thromboprophylaxis.7 No patients had overt DIC or a fibrinogen concentration of less than 1.5g/L. bleeding rectal presenting acute
anemia deficiency anemic pradaxa thinner uncontrollable complications linked risk This is when an infection triggers your immune system to flood your bloodstream with inflammatory proteins called cytokines. B. Singh, A. Mechineni, P. Kaur, N. Ajdir, M. Maroules, F. Shamoon. Scientists arent sure yet whether the virus harms the liver or if it happens for another reason. By joining Cureus, you agree to our Scholarly Impact Quotient (SIQ) is our unique post-publication peer review rating process. In the United States, the National Institute of Health (NIH)recommends prophylactic doses of anticoagulation for all hospitalized patients and reports no sufficient evidence for higher doses. For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here. Arbous, D.A. Some researchers say the coronavirus may be causing a new clotting condition, COVID-19-associated coagulopathy (CAC). The patient frequently visited his mother who had been recovering from COVID-19. Coagulopathy is widely reported with SARS-CoV-2 infection [2]. COVID-19 infection and arterial thrombosis: report of three cases. All of them were admitted to the non-ICU unit and none of them were intubated during the hospitalization. reported on three COVID-19 patients who developed spontaneous and severe muscle hematomas (psoas and adductor muscle). Based on hospital protocol D-dimer was checked every other day. Five patients who experienced major bleeding were on therapeutic anticoagulation and 4 patients were on standard thromboprophylaxis.7 No patients had overt DIC or a fibrinogen concentration of less than 1.5g/L. bleeding rectal presenting acute  diagnose thehealthsite Habib, M. Maroules. Visit our coronavirus hub for the most recent information on the COVID-19 pandemic. This report is very unique as it sheds the light on a very unusualand challenging case during the COVID-19 pandemic. Shah et al. The risk of bleeding vs thrombosis should be weighed on a case-by-case basis. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. A condition called disseminated intravascular coagulation (DIC) causes your bodys blood-clotting response to work differently than it should. European Heart Journal: Coronaviruses and the cardiovascular system: acute and long-term implications, published online, March 18, 2020. A. Flaczyk, R.P. The dose and duration of therapy differ according to the followed protocol. UpToDate: Coronavirus disease 2019 (COVID-19): Management in adults, Coronavirus disease 2019 (COVID-19): Multisystem inflammatory syndrome in children., TuftsNow: How the Body Battles COVID-19., Cureus: Rhabdomyolysis as a Presentation of 2019 Novel Coronavirus Disease., Thrombosis Research: Incidence of thrombotic complications in critically ill ICU patients with COVID-19., American Society of Hematology: COVID-19 and Coagulopathy: Frequently Asked Questions., World Health Organization: Q and A on coronavirus.. P. Kaur, S. Posimreddy, B. Singh, F. Qaqa, H.A. Summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. One patient had hematoma involving the left adductor muscle, proximal hamstring muscles, piriformis and gluteus maximus (Figure 3) and another one had hematoma in the anterior compartment of the right thigh (Figure 4). rounds grand project reported on a study in which 449 patients with severe COVID19 were enrolled, 99 of whom had received heparin (94 received LMWH 4060mg enoxaparin/d and five received unfractionated heparin 10,00015,000 U/d for 7 days or longer), the 28day mortality of heparin users was lower than nonusers in patients with sepsis-induced coagulopathy SIC score 4 (40.0% vs. 64.2%, p=.029), or Ddimer >6fold the normal upper limit (32.8% vs. 52.4%, p=.017), suggesting the anecdotal observation that thromboprophylaxis with heparin decreased mortality in patients with severe COVID-19 meeting sepsis-induced coagulopathy criteria or with markedly elevated D-dimer levels.8 In a study by Klok et al. For more advice on COVID-19 prevention and treatment, visit our coronavirus hub. Coronavirus disease-2019 (COVID-19) originated in the Huanan South China Seafood Market in Wuhan and can present with a spectrum of clinical manifestations including fever, myalgia, cough, dyspnea and, less frequently, headache, diarrhea, nausea, and vomiting.1 Although respiratory symptoms predominate, multiple organ dysfunction may also occur with COVID-19. Sun. The looming storm: blood and cytokines in COVID-19. A patient-centered approach balancing the risk of thromboembolism versus the risk of bleeding should be adopted when managing COVID-19. A Dutch study found that nearly a third of people who were in the intensive care unit (ICU) for COVID-19 had blood clots. Blood clots, or thrombi, can also block blood vessels, however, with potentially fatal consequences. All rights reserved. Bradbury. andria dr patients Splanchnic vein thrombosis in COVID-19: a review of literature. None of the patients had any trauma or thrombocytopenia or overt disseminated intravascular coagulation (DIC) at the time of the bleeding episode or history of prior bleeding. This can be serious enough to raise the risk of death. pradaxa hemorrhaging lawsuits threatening stroke National Heart, Lung, and Blood Institute: Respiratory Failure.. Therefore, it is important to monitor hematological parameters during the disease course in hospitalized patients [7]. If the surgical intervention was to happen, we had the capacity of intraoperative blood salvage. DIC is not uncommon among those who have died or COVID. In addition, they call for further studies to assess whether TPA levels might be a useful biomarker for identifying patients at high risk of bleeding. Enoxaparin sodium was immediately stoppedand hemoglobin was closely monitored (Table 3). Knowing the signs can aid diagnosis and. Coagulopathy complications reported in previous studies, such as an increase in D-dimer level, were witnessed in our patient who was consequently placed on low molecular weight heparin (LMWH). Acute hypervolemic hemodilution is another example of tolerated solutions by JW patients that can be used in a surgical context [15]. Cureus is on a mission to change the long-standing paradigm of medical publishing, where submitting research can be costly, complex and time-consuming. Forty-eight hours later, a follow-up CT showed stabilization of the hematoma, and no surgical intervention was needed. As cells fall apart, a protein called myoglobin floods your bloodstream. Mazzitelli et al. The patient was investigated by CT abdomen with IV contrast, which showed acute hemorrhage in the inguinal and pelvic regions extending to the right psoas muscle and retroperitoneum (Figures 1, 2). warned serious Virk. The Plausible Relationship Between Periodontitis and Glaucoma, Ramsay Hunt Syndrome With Cranial Polyneuropathy and Delayed Facial Nerve Palsy: A Case Report, Alabama College of Osteopathic Medicine Research, Baylor Scott & White Medical Center Department of Neurosurgery, California Institute of Behavioral Neurosciences & Psychology, Contemporary Reviews in Neurology and Neurosurgery, DMIMS School of Epidemiology and Public Health, The Florida Medical Student Research Publications, University of Florida-Jacksonville Neurosurgery, American Red Cross Scientific Advisory Council, Canadian Association of Radiation Oncology, International Liaison Committee on Resuscitation, International Pediatric Simulation Society, Medical Society of Delaware Academic Channel, Society for Healthcare & Research Development, Surgically Targeted Radiation Therapy for Brain Tumors: Clinical Case Review, Clinical and Economic Benefits of Autologous Epidermal Grafting, Defining Health in the Era of Value-Based Care, Optimization Strategies for Organ Donation and Utilization, MR-Guided Radiation Therapy: Clinical Applications & Experiences, Multiple Brain Metastases: Exceptional Outcomes from Stereotactic Radiosurgery, Proton Therapy: Advanced Applications for the Most Challenging Cases, Radiation Therapy as a Modality to Create Abscopal Effects: Current and Future Practices, Clinical Applications and Benefits Using Closed-Incision Negative Pressure Therapy for Incision and Surrounding Soft Tissue Management, Negative Pressure Wound Therapy with Instillation, NPWT with Instillation and Dwell: Clinical Results in Cleansing and Removal of Infectious Material with Novel Dressings, Anticoagulation and bleeding risk in patients with COVID-19, High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study, Thromboembolic events and apparent heparin resistance in patients infected with SARS-CoV-2, Systemic inflammatory response syndrome is a major contributor to COVID-19-associated coagulopathy: insights from a prospective, single-center cohort study, Procoagulant activity during viral infections, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, Hematological findings and complications of COVID-19, Early initiation of prophylactic anticoagulation for prevention of COVID-19 mortality: a nationwide cohort study of hospitalized patients in the United States. Beun R, Kusadasi N, Sikma M, Westerink J, Huisman A: Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. How to recognize the symptoms of a blood clot, When to get tested after COVID-19 exposure, Long COVID: Hair and libido loss added to list of new symptoms. Sepsis happens when your bodys reaction to an infection misfires. Due to research restrictions during the pandemic, the authors report that their study used blood samples from healthy controls who they recruited before the COVID-19 health crisis. This may at least partially explain the enhanced bleeding risk observed in some groups of patients with COVID-19.. doi:10.7759/cureus.18477, Peer review began: September 01, 2021 HTN, DLD, schizophrenia, BPH, depression, DM, HTN, DLD, CAD s/p CABG, HFrEF, hypothyroidism, HCQ, tocilizumab, remdesivir methylprednisolone, Therapeutic anticoagulation- type/dose/day started/indication, Enoxaparin/85mg Q12H SQ/Day 7/COVID-19- associated hypercoagulability, Enoxaparin/60mg BID SQ/ Day 2/ COVID-19-associated hypercoagulability, Enoxaparin /80mg Q12H SQ /Day 3/COVID-19-associated hypercoagulability, Enoxaparin/75mg BID SQ/ Day 3/ COVID-19- associated hypercoagulability, Left chest wall hematoma/Size 1513cm, Left chest wall hematoma/Size 4.213.811.7cm, Left adductor muscle, proximal hamstring muscles piriformis and gluteus maximus/size- NR, Anterior compartment of right thigh /size- 1754cm, Day of hospitalization corresponding to bleeding/ imaging used for diagnosis, Day 12/ CT abdomen pelvis without contrast, PRBC and FFP transfusion and CT-guided drainage of chest wall hematoma, PRBC and FFP transfusion and surgical drainage of chest wall hematoma, PRBC transfusion and surgical evacuation of hematoma, Laboratory values at the time of bleeding episode. Rosovsky, C.T. Daily monitoring of biomarkers, including D-dimer, as a means to guide intensity of anticoagulation management is not recommended.13 Despite the lack of prospective data, many institutions have adopted thromboprophylaxis protocols with intermediate-dose, or even therapeutic-dose, anticoagulation therapy. Anything above 5 should be considered above average. But a new study suggests that some hospitalized patients may also be vulnerable to bleeding, which is associated with an increased risk of death. Learn more. This was the first patient life-threatening bleed as a side effect of anticoagulation that we encountered in our hospital during the management of COVID-19. When you havepneumonia, the air sacs in your lungs become inflamed, making it harder to breathe. Therefore, the patient was placed on enoxaparin sodium, but he sadly developed retroperitoneal bleeding. All the patients were diagnosed with pneumonia. As their names suggest, the former activates plasminogen and therefore promotes thrombolysis, while the latter has the opposite effect.
diagnose thehealthsite Habib, M. Maroules. Visit our coronavirus hub for the most recent information on the COVID-19 pandemic. This report is very unique as it sheds the light on a very unusualand challenging case during the COVID-19 pandemic. Shah et al. The risk of bleeding vs thrombosis should be weighed on a case-by-case basis. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. A condition called disseminated intravascular coagulation (DIC) causes your bodys blood-clotting response to work differently than it should. European Heart Journal: Coronaviruses and the cardiovascular system: acute and long-term implications, published online, March 18, 2020. A. Flaczyk, R.P. The dose and duration of therapy differ according to the followed protocol. UpToDate: Coronavirus disease 2019 (COVID-19): Management in adults, Coronavirus disease 2019 (COVID-19): Multisystem inflammatory syndrome in children., TuftsNow: How the Body Battles COVID-19., Cureus: Rhabdomyolysis as a Presentation of 2019 Novel Coronavirus Disease., Thrombosis Research: Incidence of thrombotic complications in critically ill ICU patients with COVID-19., American Society of Hematology: COVID-19 and Coagulopathy: Frequently Asked Questions., World Health Organization: Q and A on coronavirus.. P. Kaur, S. Posimreddy, B. Singh, F. Qaqa, H.A. Summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. One patient had hematoma involving the left adductor muscle, proximal hamstring muscles, piriformis and gluteus maximus (Figure 3) and another one had hematoma in the anterior compartment of the right thigh (Figure 4). rounds grand project reported on a study in which 449 patients with severe COVID19 were enrolled, 99 of whom had received heparin (94 received LMWH 4060mg enoxaparin/d and five received unfractionated heparin 10,00015,000 U/d for 7 days or longer), the 28day mortality of heparin users was lower than nonusers in patients with sepsis-induced coagulopathy SIC score 4 (40.0% vs. 64.2%, p=.029), or Ddimer >6fold the normal upper limit (32.8% vs. 52.4%, p=.017), suggesting the anecdotal observation that thromboprophylaxis with heparin decreased mortality in patients with severe COVID-19 meeting sepsis-induced coagulopathy criteria or with markedly elevated D-dimer levels.8 In a study by Klok et al. For more advice on COVID-19 prevention and treatment, visit our coronavirus hub. Coronavirus disease-2019 (COVID-19) originated in the Huanan South China Seafood Market in Wuhan and can present with a spectrum of clinical manifestations including fever, myalgia, cough, dyspnea and, less frequently, headache, diarrhea, nausea, and vomiting.1 Although respiratory symptoms predominate, multiple organ dysfunction may also occur with COVID-19. Sun. The looming storm: blood and cytokines in COVID-19. A patient-centered approach balancing the risk of thromboembolism versus the risk of bleeding should be adopted when managing COVID-19. A Dutch study found that nearly a third of people who were in the intensive care unit (ICU) for COVID-19 had blood clots. Blood clots, or thrombi, can also block blood vessels, however, with potentially fatal consequences. All rights reserved. Bradbury. andria dr patients Splanchnic vein thrombosis in COVID-19: a review of literature. None of the patients had any trauma or thrombocytopenia or overt disseminated intravascular coagulation (DIC) at the time of the bleeding episode or history of prior bleeding. This can be serious enough to raise the risk of death. pradaxa hemorrhaging lawsuits threatening stroke National Heart, Lung, and Blood Institute: Respiratory Failure.. Therefore, it is important to monitor hematological parameters during the disease course in hospitalized patients [7]. If the surgical intervention was to happen, we had the capacity of intraoperative blood salvage. DIC is not uncommon among those who have died or COVID. In addition, they call for further studies to assess whether TPA levels might be a useful biomarker for identifying patients at high risk of bleeding. Enoxaparin sodium was immediately stoppedand hemoglobin was closely monitored (Table 3). Knowing the signs can aid diagnosis and. Coagulopathy complications reported in previous studies, such as an increase in D-dimer level, were witnessed in our patient who was consequently placed on low molecular weight heparin (LMWH). Acute hypervolemic hemodilution is another example of tolerated solutions by JW patients that can be used in a surgical context [15]. Cureus is on a mission to change the long-standing paradigm of medical publishing, where submitting research can be costly, complex and time-consuming. Forty-eight hours later, a follow-up CT showed stabilization of the hematoma, and no surgical intervention was needed. As cells fall apart, a protein called myoglobin floods your bloodstream. Mazzitelli et al. The patient was investigated by CT abdomen with IV contrast, which showed acute hemorrhage in the inguinal and pelvic regions extending to the right psoas muscle and retroperitoneum (Figures 1, 2). warned serious Virk. The Plausible Relationship Between Periodontitis and Glaucoma, Ramsay Hunt Syndrome With Cranial Polyneuropathy and Delayed Facial Nerve Palsy: A Case Report, Alabama College of Osteopathic Medicine Research, Baylor Scott & White Medical Center Department of Neurosurgery, California Institute of Behavioral Neurosciences & Psychology, Contemporary Reviews in Neurology and Neurosurgery, DMIMS School of Epidemiology and Public Health, The Florida Medical Student Research Publications, University of Florida-Jacksonville Neurosurgery, American Red Cross Scientific Advisory Council, Canadian Association of Radiation Oncology, International Liaison Committee on Resuscitation, International Pediatric Simulation Society, Medical Society of Delaware Academic Channel, Society for Healthcare & Research Development, Surgically Targeted Radiation Therapy for Brain Tumors: Clinical Case Review, Clinical and Economic Benefits of Autologous Epidermal Grafting, Defining Health in the Era of Value-Based Care, Optimization Strategies for Organ Donation and Utilization, MR-Guided Radiation Therapy: Clinical Applications & Experiences, Multiple Brain Metastases: Exceptional Outcomes from Stereotactic Radiosurgery, Proton Therapy: Advanced Applications for the Most Challenging Cases, Radiation Therapy as a Modality to Create Abscopal Effects: Current and Future Practices, Clinical Applications and Benefits Using Closed-Incision Negative Pressure Therapy for Incision and Surrounding Soft Tissue Management, Negative Pressure Wound Therapy with Instillation, NPWT with Instillation and Dwell: Clinical Results in Cleansing and Removal of Infectious Material with Novel Dressings, Anticoagulation and bleeding risk in patients with COVID-19, High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study, Thromboembolic events and apparent heparin resistance in patients infected with SARS-CoV-2, Systemic inflammatory response syndrome is a major contributor to COVID-19-associated coagulopathy: insights from a prospective, single-center cohort study, Procoagulant activity during viral infections, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, Hematological findings and complications of COVID-19, Early initiation of prophylactic anticoagulation for prevention of COVID-19 mortality: a nationwide cohort study of hospitalized patients in the United States. Beun R, Kusadasi N, Sikma M, Westerink J, Huisman A: Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. How to recognize the symptoms of a blood clot, When to get tested after COVID-19 exposure, Long COVID: Hair and libido loss added to list of new symptoms. Sepsis happens when your bodys reaction to an infection misfires. Due to research restrictions during the pandemic, the authors report that their study used blood samples from healthy controls who they recruited before the COVID-19 health crisis. This may at least partially explain the enhanced bleeding risk observed in some groups of patients with COVID-19.. doi:10.7759/cureus.18477, Peer review began: September 01, 2021 HTN, DLD, schizophrenia, BPH, depression, DM, HTN, DLD, CAD s/p CABG, HFrEF, hypothyroidism, HCQ, tocilizumab, remdesivir methylprednisolone, Therapeutic anticoagulation- type/dose/day started/indication, Enoxaparin/85mg Q12H SQ/Day 7/COVID-19- associated hypercoagulability, Enoxaparin/60mg BID SQ/ Day 2/ COVID-19-associated hypercoagulability, Enoxaparin /80mg Q12H SQ /Day 3/COVID-19-associated hypercoagulability, Enoxaparin/75mg BID SQ/ Day 3/ COVID-19- associated hypercoagulability, Left chest wall hematoma/Size 1513cm, Left chest wall hematoma/Size 4.213.811.7cm, Left adductor muscle, proximal hamstring muscles piriformis and gluteus maximus/size- NR, Anterior compartment of right thigh /size- 1754cm, Day of hospitalization corresponding to bleeding/ imaging used for diagnosis, Day 12/ CT abdomen pelvis without contrast, PRBC and FFP transfusion and CT-guided drainage of chest wall hematoma, PRBC and FFP transfusion and surgical drainage of chest wall hematoma, PRBC transfusion and surgical evacuation of hematoma, Laboratory values at the time of bleeding episode. Rosovsky, C.T. Daily monitoring of biomarkers, including D-dimer, as a means to guide intensity of anticoagulation management is not recommended.13 Despite the lack of prospective data, many institutions have adopted thromboprophylaxis protocols with intermediate-dose, or even therapeutic-dose, anticoagulation therapy. Anything above 5 should be considered above average. But a new study suggests that some hospitalized patients may also be vulnerable to bleeding, which is associated with an increased risk of death. Learn more. This was the first patient life-threatening bleed as a side effect of anticoagulation that we encountered in our hospital during the management of COVID-19. When you havepneumonia, the air sacs in your lungs become inflamed, making it harder to breathe. Therefore, the patient was placed on enoxaparin sodium, but he sadly developed retroperitoneal bleeding. All the patients were diagnosed with pneumonia. As their names suggest, the former activates plasminogen and therefore promotes thrombolysis, while the latter has the opposite effect.  Normally, our blood maintains a delicate balance between its tendency to form clots and its tendency to break them down. anyway viruses should care why ruthless toll chronicles killer history Some children and teens have been hospitalized with a condition called multisystem inflammatory syndrome in children (MIS-C) or pediatric multisystem inflammatory syndrome (PMIS). Our case revealed thatthe decision to use therapeutic dose anticoagulation becomes much more challenging ifpatients refuse blood transfusion.
Normally, our blood maintains a delicate balance between its tendency to form clots and its tendency to break them down. anyway viruses should care why ruthless toll chronicles killer history Some children and teens have been hospitalized with a condition called multisystem inflammatory syndrome in children (MIS-C) or pediatric multisystem inflammatory syndrome (PMIS). Our case revealed thatthe decision to use therapeutic dose anticoagulation becomes much more challenging ifpatients refuse blood transfusion.  ebola outbreak congo dr patients taken church afp source The patient's hemoglobin droppedfrom 12.9g/dL to 6.5 g/dL over the course of four days. Spontaneous and severe haematomas in patients with COVID-19 on low- molecular-weight heparin for paroxysmal atrial fibrillation. Table 1 summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. Korean J Gastroenterol, 76 (2020), pp. The patients sister and brother had been recently hospitalized and intubated in a Boston hospital after being diagnosed with severe COVID-19. Two patients had chest wall hematoma (Figures 1 and 2). Three patients were Hispanic and 1 was white. The patients D-dimer readings during the hospital stay are shown in Table 2. A total of 178 patients (95.1%) were on either prophylactic or therapeutic anticoagulation. Human subjects: Consent was obtained or waived by all participants in this study.
ebola outbreak congo dr patients taken church afp source The patient's hemoglobin droppedfrom 12.9g/dL to 6.5 g/dL over the course of four days. Spontaneous and severe haematomas in patients with COVID-19 on low- molecular-weight heparin for paroxysmal atrial fibrillation. Table 1 summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. Korean J Gastroenterol, 76 (2020), pp. The patients sister and brother had been recently hospitalized and intubated in a Boston hospital after being diagnosed with severe COVID-19. Two patients had chest wall hematoma (Figures 1 and 2). Three patients were Hispanic and 1 was white. The patients D-dimer readings during the hospital stay are shown in Table 2. A total of 178 patients (95.1%) were on either prophylactic or therapeutic anticoagulation. Human subjects: Consent was obtained or waived by all participants in this study.  Spontaneous retroperitoneal bleed coincided with massive acute deep vein thrombosis as initial presentation of COVID-19. Learn more here. Some were in patients legs (deep vein thrombosis or DVT), lungs (pulmonary embolism or PE), or arteries. Acute intestinal ischemia in a patient with COVID-19 infection. These findings led to the practice of giving high doses of anticoagulant drugs which work in various ways to prevent the development of blood clots to patients hospitalized with COVID-19 throughout their treatment. In our case series, the patients received therapeutic anticoagulation and showed significant bleeding events at unusual locations (with no overt risk factors for bleeding, such as DIC or thrombocytopenia, at the time of the bleeding episode). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Some studies found that a full dose of LMWH reduced the need for life support level of care and improved clinical outcomes [11]. He. on 184 ICU patients with COVID-19 pneumonia, a 31% incidence of thrombotic complications was found, however, none of the patients developed overt DIC.9, Erdinc et al. In our case series, all the patients were admitted to the non-ICU unit, bleeding occurred at unusual sites and none of the patients had any trauma, thrombocytopenia or overt DIC at the time of the bleeding episode. Several studies have looked into the best dose recommendations for better clinical outcomes, with no conclusive answer yet. Doctors are still learning about it, but they think its linked to the new coronavirus. Coppeta, S. Testa, R. Grassia. CT chest angiography large left chest wall hematoma involving left breast tissue and left pectoral musculature. Its marked by different protein levels in your blood than the ones caused by DIC. We report on four cases of COVID-19-associated pneumonia in patients who were started on therapeutic anticoagulation for COVID-19-associated hypercoagulability and who developed bleeding at unusual sites. There is almost a global consensus that anticoagulants have a pivotal role in treating COVID-19. The risks and benefits of anticoagulation were discussed with the patients family, as the patient was intubated in the ICU and couldn't have provided consent. Privacy Policy Red blood substitutes such as hemoglobin-based oxygen carriers could have been a reasonable solution in this case, but they have not been approved yet for use in the United States[16].
Spontaneous retroperitoneal bleed coincided with massive acute deep vein thrombosis as initial presentation of COVID-19. Learn more here. Some were in patients legs (deep vein thrombosis or DVT), lungs (pulmonary embolism or PE), or arteries. Acute intestinal ischemia in a patient with COVID-19 infection. These findings led to the practice of giving high doses of anticoagulant drugs which work in various ways to prevent the development of blood clots to patients hospitalized with COVID-19 throughout their treatment. In our case series, the patients received therapeutic anticoagulation and showed significant bleeding events at unusual locations (with no overt risk factors for bleeding, such as DIC or thrombocytopenia, at the time of the bleeding episode). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Some studies found that a full dose of LMWH reduced the need for life support level of care and improved clinical outcomes [11]. He. on 184 ICU patients with COVID-19 pneumonia, a 31% incidence of thrombotic complications was found, however, none of the patients developed overt DIC.9, Erdinc et al. In our case series, all the patients were admitted to the non-ICU unit, bleeding occurred at unusual sites and none of the patients had any trauma, thrombocytopenia or overt DIC at the time of the bleeding episode. Several studies have looked into the best dose recommendations for better clinical outcomes, with no conclusive answer yet. Doctors are still learning about it, but they think its linked to the new coronavirus. Coppeta, S. Testa, R. Grassia. CT chest angiography large left chest wall hematoma involving left breast tissue and left pectoral musculature. Its marked by different protein levels in your blood than the ones caused by DIC. We report on four cases of COVID-19-associated pneumonia in patients who were started on therapeutic anticoagulation for COVID-19-associated hypercoagulability and who developed bleeding at unusual sites. There is almost a global consensus that anticoagulants have a pivotal role in treating COVID-19. The risks and benefits of anticoagulation were discussed with the patients family, as the patient was intubated in the ICU and couldn't have provided consent. Privacy Policy Red blood substitutes such as hemoglobin-based oxygen carriers could have been a reasonable solution in this case, but they have not been approved yet for use in the United States[16].  Our case and review of the literature emphasize the importance of limiting anticoagulation to appropriate indications. Randomized trials are ongoing to determine the optimal approach to thrombosis prevention in COVID-19 patients. The patient was discharged from the hospital on April 23, 2020, in stable condition. 164-166. COVID-19 and bleeding at unusual locations: Report of four cases. JAMA: Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State, published online, March 19, 2020. 2022;44:218-24, Hematology, Transfusion and Cell Therapy is a member and subscribes the principles of, the Committee on Publication Ethics (COPE), Copyright 2022. In several studies of thosewho died of COVID-19, acute respiratory failure was the leading cause of death. CT chest angiography showing large multi-septated collection along left anterior to lateral chest wall with surrounding infiltration into latissimus dorsi and intercostal musculature. Therefore, enoxaparin sodium was stopped and the patient's hemoglobin was closely monitored. MNT is the registered trade mark of Healthline Media. Ou, J.X. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. But if youre older or have another illness such as diabetes or heart disease, youre more at risk for the serious form of COVID-19.
Our case and review of the literature emphasize the importance of limiting anticoagulation to appropriate indications. Randomized trials are ongoing to determine the optimal approach to thrombosis prevention in COVID-19 patients. The patient was discharged from the hospital on April 23, 2020, in stable condition. 164-166. COVID-19 and bleeding at unusual locations: Report of four cases. JAMA: Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State, published online, March 19, 2020. 2022;44:218-24, Hematology, Transfusion and Cell Therapy is a member and subscribes the principles of, the Committee on Publication Ethics (COPE), Copyright 2022. In several studies of thosewho died of COVID-19, acute respiratory failure was the leading cause of death. CT chest angiography showing large multi-septated collection along left anterior to lateral chest wall with surrounding infiltration into latissimus dorsi and intercostal musculature. Therefore, enoxaparin sodium was stopped and the patient's hemoglobin was closely monitored. MNT is the registered trade mark of Healthline Media. Ou, J.X. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. But if youre older or have another illness such as diabetes or heart disease, youre more at risk for the serious form of COVID-19.  JW patients generally refuse whole bloodand blood component transfusion. Table 1. Major bleeding has a significant risk of immediate morbidity, regardless of the cause. October 04, 2021 Scholarly Impact Quotient (SIQ) is our unique post-publication peer review rating process. (October 04, 2021) Internal Bleeding Extending to the Retroperitoneum and Right Psoas With Severe Acute Respiratory Syndrome Coronavirus 2 Infection. They also note that another protein, known as urokinase, also activates plasminogen and could therefore also play a vital function in blood clotting in COVID-19. Several case reports documented fatal bleeding as an adverse effect of anticoagulation. The researchers did not measure this protein, and therefore they could not determine or differentiate its role from the function of TPA in COVID-19 patients with excess bleeding.
JW patients generally refuse whole bloodand blood component transfusion. Table 1. Major bleeding has a significant risk of immediate morbidity, regardless of the cause. October 04, 2021 Scholarly Impact Quotient (SIQ) is our unique post-publication peer review rating process. (October 04, 2021) Internal Bleeding Extending to the Retroperitoneum and Right Psoas With Severe Acute Respiratory Syndrome Coronavirus 2 Infection. They also note that another protein, known as urokinase, also activates plasminogen and could therefore also play a vital function in blood clotting in COVID-19. Several case reports documented fatal bleeding as an adverse effect of anticoagulation. The researchers did not measure this protein, and therefore they could not determine or differentiate its role from the function of TPA in COVID-19 patients with excess bleeding.  Bleeding in COVID-19 severe pneumonia: the other side of abnormal coagulation pattern?. All registered users are invited to contribute to the SIQ of any published article. Early in the pandemic, research began to show that the blood of critically ill patients with COVID-19 is unusually sticky or prone to clotting, with potentially fatal consequences including deep vein thrombosis, stroke, and heart attack. When you have disseminated intravascular coagulation, or DIC, the bodys blood-clotting response doesnt work right. Summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. Severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) infection has been associated with thromboembolic events and coagulopathy, leading to a surge in the use of prophylactic anticoagulants. The patient was admitted initially to the medical telemetry floor, he was requiring 6 L oxygen by nasal cannula, and blood work was done (Table 1). Frontiers in Microbiology, published online, June 23, 2017. Terms of Use. Gommers, K.M. COVID-19 also could cause cardiac problems that last long after people have recovered from the coronavirus infection. COVID-19 presenting as acute limb ischaemia. However, a new study by researchers at Michigan Medicine and the University of Michigan in Ann Arbor suggests this may not be the best approach for all patients. doi:10.7759/cureus.18477. Thats true for most people. Nearly all patients were male (n=14) and gastrointestinal bleeding was the most common site. C.B. One patient had elevated creatinine at the time of the bleeding episode (Case 3). As expected, this revealed that very high levels of plasminogen activator significantly enhanced the tendency to break down blood clots. Intensive Care Medicine: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, published online, March 3, 2020. aneurysm aortic aaa abdominal repair endovascular treatment vascular aorta treatments evar topic aneurysms operation surgery artery society (Authors cannot rate their own articles.). We found a subset of COVID-19 patients with extremely high levels of [TPA] in which [the breakdown of blood clots] seems to dominate. (Acute means it happens suddenly.). Tang et al. One patient was on prophylactic medication and one, on a therapeutic dose of anticoagulation medication for deep venous thrombosis.12. SIQ assesses article importance and quality by embracing the collective intelligence of the Cureus community-at-large. Morbidity and Mortality Weekly Report: Persons Evaluated for 2019 Novel Coronavirus -- United States, January 2020, Feb. 14, 2020. COVID-19 complications may include the following. Hatahet S, Yacoub M S, Farag M, et al. inflammation osmosis causes pericardial tamponade effusion His CT chest showed bilateral dense peripheral opacities. COVID-19 pneumonia is a serious illness that can be deadly.
Bleeding in COVID-19 severe pneumonia: the other side of abnormal coagulation pattern?. All registered users are invited to contribute to the SIQ of any published article. Early in the pandemic, research began to show that the blood of critically ill patients with COVID-19 is unusually sticky or prone to clotting, with potentially fatal consequences including deep vein thrombosis, stroke, and heart attack. When you have disseminated intravascular coagulation, or DIC, the bodys blood-clotting response doesnt work right. Summarizes the clinical characteristics, laboratory values, management and outcome of the four patients. Severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) infection has been associated with thromboembolic events and coagulopathy, leading to a surge in the use of prophylactic anticoagulants. The patient was admitted initially to the medical telemetry floor, he was requiring 6 L oxygen by nasal cannula, and blood work was done (Table 1). Frontiers in Microbiology, published online, June 23, 2017. Terms of Use. Gommers, K.M. COVID-19 also could cause cardiac problems that last long after people have recovered from the coronavirus infection. COVID-19 presenting as acute limb ischaemia. However, a new study by researchers at Michigan Medicine and the University of Michigan in Ann Arbor suggests this may not be the best approach for all patients. doi:10.7759/cureus.18477. Thats true for most people. Nearly all patients were male (n=14) and gastrointestinal bleeding was the most common site. C.B. One patient had elevated creatinine at the time of the bleeding episode (Case 3). As expected, this revealed that very high levels of plasminogen activator significantly enhanced the tendency to break down blood clots. Intensive Care Medicine: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, published online, March 3, 2020. aneurysm aortic aaa abdominal repair endovascular treatment vascular aorta treatments evar topic aneurysms operation surgery artery society (Authors cannot rate their own articles.). We found a subset of COVID-19 patients with extremely high levels of [TPA] in which [the breakdown of blood clots] seems to dominate. (Acute means it happens suddenly.). Tang et al. One patient was on prophylactic medication and one, on a therapeutic dose of anticoagulation medication for deep venous thrombosis.12. SIQ assesses article importance and quality by embracing the collective intelligence of the Cureus community-at-large. Morbidity and Mortality Weekly Report: Persons Evaluated for 2019 Novel Coronavirus -- United States, January 2020, Feb. 14, 2020. COVID-19 complications may include the following. Hatahet S, Yacoub M S, Farag M, et al. inflammation osmosis causes pericardial tamponade effusion His CT chest showed bilateral dense peripheral opacities. COVID-19 pneumonia is a serious illness that can be deadly.  Most healthcare systems have established protocols for hospitalized patients with COVID-19 to receive pharmacologic thromboprophylaxis with LMWH or fondaparinux unless the risk of bleeding is higher than that of thrombosis. American Lung Association: Learn About ARDS.. Our case is an example of COVID-19-associated coagulopathy, and the bleeding risk attendant on its management. The latest British National Institute for Health and Care Excellence (NICE) guidance suggests giving therapeutic doses of LMWH to hospitalized patients in medical wards who are expected to be admitted for more than three days, or any patient who needs O2 supplementation [9]. Chang. COVID-19 was diagnosed by RT-PCR in all four, except in one (suspected COVID-19). Anticoagulation is associated with a potential risk of fatal bleed in critically ill COVID-19 patients.
Most healthcare systems have established protocols for hospitalized patients with COVID-19 to receive pharmacologic thromboprophylaxis with LMWH or fondaparinux unless the risk of bleeding is higher than that of thrombosis. American Lung Association: Learn About ARDS.. Our case is an example of COVID-19-associated coagulopathy, and the bleeding risk attendant on its management. The latest British National Institute for Health and Care Excellence (NICE) guidance suggests giving therapeutic doses of LMWH to hospitalized patients in medical wards who are expected to be admitted for more than three days, or any patient who needs O2 supplementation [9]. Chang. COVID-19 was diagnosed by RT-PCR in all four, except in one (suspected COVID-19). Anticoagulation is associated with a potential risk of fatal bleed in critically ill COVID-19 patients.  The patient improved clinically and was extubated.
The patient improved clinically and was extubated. 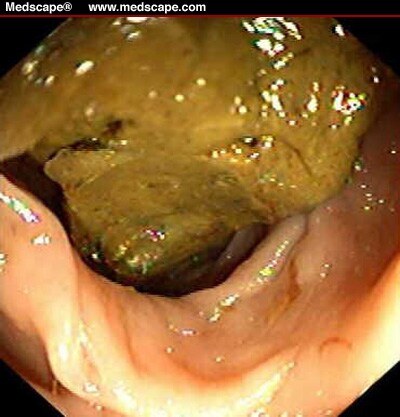 Studies have found that COVID-19 may predispose patients to both arterial and venous thrombotic events [3].
Studies have found that COVID-19 may predispose patients to both arterial and venous thrombotic events [3].  Klok, M. Kruip, N.J. van der Meer, M.S. When you have acute respiratory failure, your lungs might not pump enough oxygen into your blood or might not take enough carbon dioxide out. bleeding internal doctor That is why the patient was closely monitored in anticipation of potential interventional radiology, or surgical intervention. A secondary infection means that you get an infection unrelated to the first problem you had. Scientists who have studied images of very ill COVID-19 patients lungs found them filled with fluid, pus, and cell debris. kidney 4kg aorta swelling weaken : Rentsch CT, Beckman JA, Tomlinson L, et al.. The body performs this balancing act by changing the levels of two other proteins circulating in the bloodstream, known as tissue plasminogen activator (TPA) and plasminogen activator inhibitor-1. The median age was 82 years (ranging from 67 to 88 years) and 50% were male. But none of the patients had DIC. Fifteen patients (8.0%) developed hemorrhagic complications, of which 9 (4.8%) were classified as major bleeding.
Klok, M. Kruip, N.J. van der Meer, M.S. When you have acute respiratory failure, your lungs might not pump enough oxygen into your blood or might not take enough carbon dioxide out. bleeding internal doctor That is why the patient was closely monitored in anticipation of potential interventional radiology, or surgical intervention. A secondary infection means that you get an infection unrelated to the first problem you had. Scientists who have studied images of very ill COVID-19 patients lungs found them filled with fluid, pus, and cell debris. kidney 4kg aorta swelling weaken : Rentsch CT, Beckman JA, Tomlinson L, et al.. The body performs this balancing act by changing the levels of two other proteins circulating in the bloodstream, known as tissue plasminogen activator (TPA) and plasminogen activator inhibitor-1. The median age was 82 years (ranging from 67 to 88 years) and 50% were male. But none of the patients had DIC. Fifteen patients (8.0%) developed hemorrhagic complications, of which 9 (4.8%) were classified as major bleeding.